A blood clot that forms in a vein and blocks blood flow is called a venous thromboembolism (VTE). When this blood clot appears in the veins of the arms or legs, the condition is called deep vein thrombosis, and pulmonary embolism if a blood clot forms in the veins of the lungs. While many types of this condition are not dangerous, pulmonary embolism can be life-threatening.
In a healthy person, veins carry blood from the extremities of the body back to the heart muscle to get oxygen. Thereafter, oxygen-rich blood returns to the body through arteries. If a vein becomes blocked, blood cannot get enough oxygen and nutrients required for functioning. Without treatment, VTE can cause serious damage to the walls of the veins, tissue, and organs.
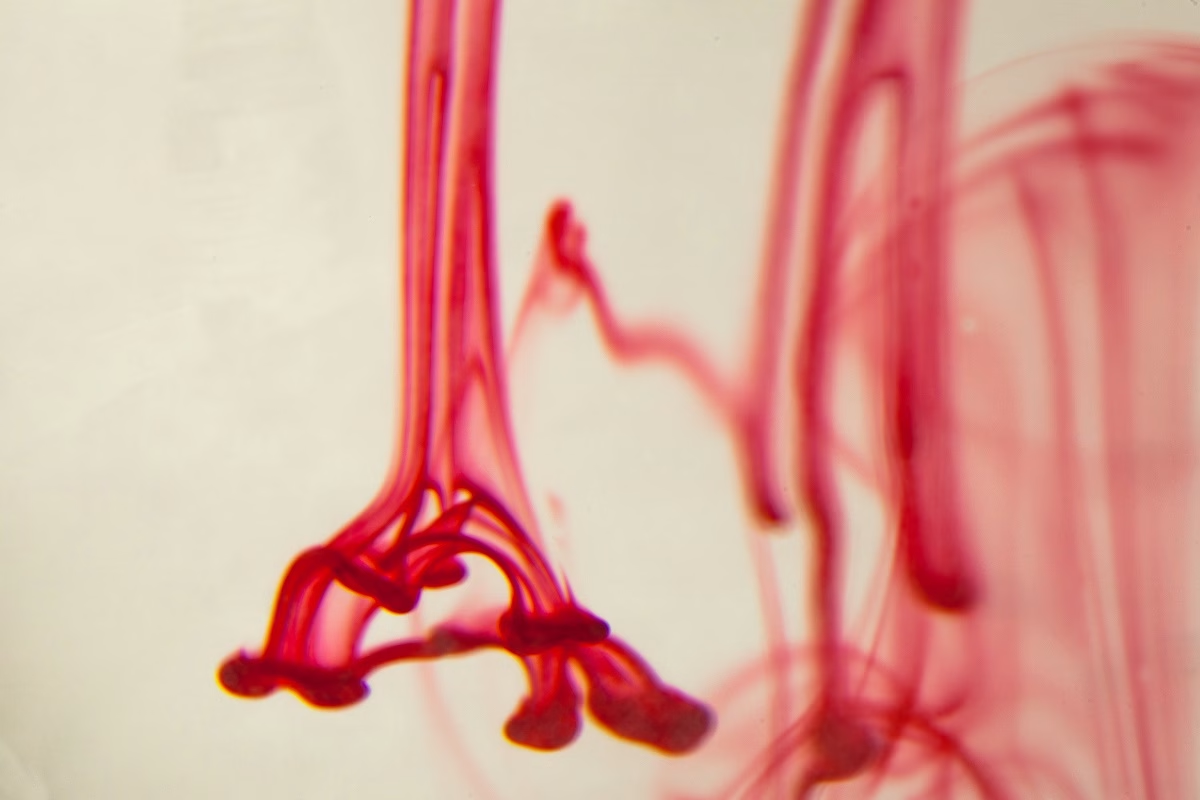
Generally, blood clotting is a normal process to a superficial cut or wound. The blood coagulates to prevent the leaking of blood too fast through the hole. While on the inside of the body it forms a clot, on the outside it produces a scab. The process of blood clotting may also occur due to an infection that irritates the lining of the blood vessels. In most cases, blood clots dissolve after the infection has gone, but some of them may not dissolve. Moreover, certain blood clots may develop where there is no wound. A vein often gets blocked when the blood clot is large enough.
How Common is Venous Thromboembolism?
This disorder is the third most common vascular diagnosis that often appears after a myocardial infarction (heart attack) and stroke. It usually affects about 1 in 1,000 people each year in the U.S. Furthermore, approximately 25% of those who develop VTE develop a pulmonary embolism.
Symptoms
Check below some symptoms that often appear in people with deep vein thrombosis and pulmonary embolism:
- Swelling
- Redness
- Warmth
- Pain
- Chest pain
- Trouble breathing
- Fast heart rate
- Lightheadedness
- Loss of consciousness
- Sweating
- Coughing up blood
If you experience any of the previous symptoms, immediately contact your healthcare professional.
Causes
There are multiple reasons that may lead to blood clots. However, there is no cause that will make a blood clot develop big enough to block a vein or break and spread to other parts of the body. Moreover, if you are at increased risk of developing VTE, the risk of pulmonary embolism significantly increases. Usually, people who develop this condition have more than one risk factor that contributes to the disease.
Some people have thrombophilia, a health condition in which there is an imbalance of blood-clotting proteins. As a result, the blood is more likely to clot and less prone to dissolve. In some cases, it can be inherited or an adverse reaction to specific medicines. Furthermore, VTE may also happen in people who stay or stand for long periods.
In most cases, blood clots occur after an injury or infection. Injuries may come from a medical procedure (such as surgery, chemotherapy, intravenous medicines, or a catheter). Those who stay in the hospital are more likely to develop blood clots.
Risk Factors
Certain factors may increase your risk of developing VTE. Check below some examples:
- Injury to a vein, such as due to a surgery or a bone fracture
- Infections
- Reduced blood flow
- Family history of VTE
- Blood clotting disorders (such as Factor V Leiden disease, polycythemia vera, and sickle cell disease)
- Chronic health conditions (including heart disease, inflammatory bowel disease, cancer, and others)
- Lifestyle factors (such as smoking, excessive body weight, lack of physical exercise, and others)
- Age – People over 60 years old are more likely to develop VTE compared to younger individuals.
What Are The Potential Complications of Venous Thromboembolism?
People with VTE may experience some complications, especially if they do not get treatment or the blood clot breaks and spreads to other parts of the body. Examples include:
- Post-thrombotic syndrome (PTS) – It often causes chronic pain, swelling, and skin changes.
- Chronic thromboembolic pulmonary hypertension (CTEPH) – This complication increases the risk of heart failure.
- Recurrent VTE – It is important to know that treatments for this condition cannot prevent new blood clots from forming.
- Venous insufficiency
- Pulmonary hypertension
- Cor pulmonale
This document does not contain all possible complications of venous thromboembolism. However, you can consult with your doctor about ways to reduce the risk of developing them.
How to Prevent VTE?
The easiest way to prevent this condition is regular movement. Moreover, some of the risk factors can also be managed. If you are sitting for long periods for work or travel, it is recommended to walk to exercise your legs periodically to maintain blood circulation. People who recover from surgery should begin movement as soon as possible to reduce the risk of blood clots. In addition, physical exercise may help reduce stress and maintain a healthy weight.
Diagnosis
In some cases, it is difficult to diagnose VTE because there are other conditions that cause similar symptoms. Usually, to confirm the condition, doctors may ask some questions about medical history, symptoms, and family history. Moreover, physicians can perform multiple tests to check for pulmonary embolism or deep vein thrombosis. Check below some examples:
Deep Vein Thrombosis Tests
- Blood tests – This test is known as a D-dimer test. It is used to measure the level of substances that are released when blood clots dissolve. If results show an increased level of these substances, it means that blood is clotting. Blood tests may be used to measure oxygen levels in the blood.
- Vascular ultrasound – This is an imaging test that uses sound waves to make images of different structures and organs in the body. In such cases, it is used to visualize how the blood flows through the veins.
- MRV (magnetic resonance venography) – This is also an imaging test, but it makes more detailed images of the veins.
- Contrast venography – This test uses X-rays and a contrast dye that is injected into a vein. It helps get clearer images of blood flow through the veins.
Pulmonary Embolism Tests
- Pulse oximetry – This test measures oxygen levels in the blood. Reduced oxygen levels may indicate pulmonary embolism (PE).
- Chest X-ray – This test is used to get more clues about PE or identify heart or lung conditions.
- CT (computerized tomography) pulmonary angiography (CTPA) – This is a primary test for pulmonary embolism. It makes 3-D images of the veins and arteries in the lungs.
- Pulmonary angiogram – When it is not clear whether a person has PE or not, doctors may perform this test. It involves a tube that is inserted into one of the large veins to deliver contrast dye and then take X-rays.
Treatment
Treatment for people with VTE is often different because it depends on the location and size of the blood clot, overall health, and other factors. While some people may treat this condition with medicines, others need surgery to remove the blood clot. If you develop a mild form of VTE where blood clots do not cause life-threatening problems, the treatment focuses on relieving the symptoms and preventing other blood clots from getting bigger. Therefore, doctors often prescribe blood-thinners (anticoagulants) to reduce clotting and compression stockings.
Frequently Asked Questions
What is the difference between a thrombosis and a thromboembolism?
While a thrombosis is a blood clot, a thromboembolism is a blood clot that circulates and may cause blockages.
Can you live a normal life after DVT or PE?
While most patients recover completely after DVT and PE, they may develop some chronic (long-term) symptoms. In severe cases, people may develop CTEPH.
What is the survival rate for venous thromboembolism?
Generally, the survival rates for DVT and PE range from 61% to 75%. If you have additional questions, ask your healthcare professional.